5 Tips to Better Communicate With Your Personal Injury Patients
Dr. Tauber is the COO and Director of Education at the American Institute of Personal Injury Physicians. He has over 30 years of experience in both healthcare practice and consulting. A sought-after national guest speaker at med-legal conferences and state association events, he has also been published in national journals. Dr. Tauber is the creator of the “Personal Injury Success Blueprint System” designed to help providers overcome their PI obstacles and quickly improve success.

In my previous blog, I identified four principles to help you connect with your personal injury (PI) patients. These were empathy, listening, time, communication, and understanding.
In addition, I described how these will continually intertwine throughout your PI cases.
In this segment, those same four principles will be applied to one of the most important aspects of PI cases, the initial knee-to-knee patient history.
The initial story becomes the first opportunity for you as the treating provider to connect with your patient. If you recall from the first segment, the majority of the patient connection foundation was created by the office team members. This happened through the initial patient procedures including the phone call, office forms, and other pre-first visit office procedures.
1. Information Breakdown For Your Patient’s

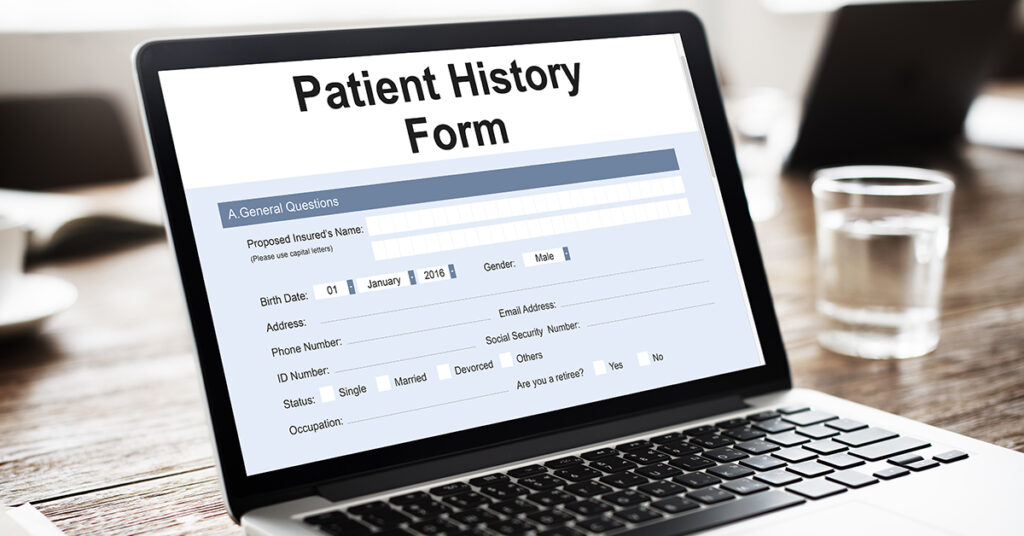
Before entering the room to introduce yourself, take a few moments and review the patient’s completed initial forms. This will help to gain a clearer understanding of the patient’s trauma, injuries, and post-injury treatment. Here’s what to look for, the accident description, mechanism of trauma, type and amount of current, and other post-injury symptoms.
Another area to take a look at is the patient’s compliance with completing the intake documents. Many times, the manner in which documents are completed can give insight into the patient’s injuries, especially traumatic brain injury or concussions.
This includes handwriting, the transposing of dates or information. Take note of spelling and any areas of documents that are missing, skipped, or not completed correctly. Both of these actions represent step one in your new patient connection process.
In addition, the entire process may seem routine to someone like yourself, (accustomed to PI cases). However, the experience most likely is very upsetting and disturbing for your patient.
For your patients, their case can be filled with many new and unfamiliar factors and variables. Especially if this is their first accident or injury or if it was particularly violent, injurious, or life-changing. Having empathy for your patients is key towards helping your patients on their road to recovery.
2. Listening Is Key
After initial introductions are over, now you want to spend an appropriate amount of time with your patient actively listening to their story of the events. Adequate time is not only necessary to connect, but for a complete clinical picture. Many providers approach the new patient history as an obligation, and even some with an “I’ve seen these injuries or cases before attitude.” Avoiding the “I know how this is going to go” mindset is crucial for a strong patient connection.
There have been studies that show in many cases providers diagnosed their patients within 10 minutes. This mentality is not beneficial at any time, but especially in trauma cases. Even minor traumas, impacts, or injuries can have potentially devastating, long-term, or even permanent consequences. One of the biggest complaints patients have with providers in today’s busy environment is they don’t take the time to listen to them.
The act of listening is a significant aspect of the initial patient history. Listen intently to the words the patient uses, how they describe their symptoms and pain. If you incorporate pain scales in the documentation, listen to the numbers a patient chooses to communicate their pain levels. It can give you an understanding of the patient and their current symptoms.
3. Pros And Cons Of Pain Scales
The use of pain scales can be both beneficial and problematic in personal injury cases. The reporting of high pain scales during the initial history can be interpreted in several different ways.
One way is it’s only indicative of the patient’s attempt to communicate they are “really hurt” and not an accurate depiction. This type of potentially inaccurate pain reporting can occur when the scale is missing an underlying component. Without objectifying, any number(s) a patient chooses will at best just be random, basically, a number picked out of “thin air.”
High patient pain scales can also carry consequences. High numbers imply the patient should either be medically evaluated in an emergency setting such as an Urgent Care or hospital emergency department.
Review any pain scale prior to implementation into your cases. Be sure there is a way to objectify the number(s) of any scale chosen. There are options available, including using a 10-centimeter line with minimal patient encouragement. Even a visual analog scale such as the Wong-Baker or other similar scales.
There are studies indicating providers need to appreciate the potential for error when using pain scales. In sum, the interpretation of the patient responses may not be as straightforward as it appears.
4. Improve Your Body Language

Listening during the patient’s history also involves the use of body language. The simple act of leaning forward, towards the patient is a non-verbal way of demonstrating your engagement.
Another is nodding your head as the patient relates their crash experience and injuries. These subtle body language cues can often be overlooked during the course of a busy day with other office visits.
In addition, try to avoid interrupting the patient as they report their history. Unless there is a specific follow-up question or a certain point that requires clarification.
Try to allow the patient to fully complete their history, then go back for specific questions and clarification. This can help to keep the patient-focused and result in a more accurate recall of events.
5. How Else Can You Help?
Once everything has been recorded and documented make sure to repeat the entire patient’s history back to them. Nothing says “I was listening and understanding” more so than repeating an entire patient history. This truly can solidify your connection to your patients.
Take a couple of steps further by asking the patient “is there anything that you (the provider) missed?” A good question to also ask your personal injury patients is, “Is there anything else they feel is important they would like to add that you did not ask?”
There are personal injury-specific reasons for adding these last two questions. First, it ensures the patient has an opportunity to take a moment and think about everything that has happened to them since the injury. This is critical for the reporting of a patient history that is complete, thorough, and consistent. Patient inconsistencies, even unintentional ones can become a problem later on in cases.
Next, there may be patient issues or concerns outside their history. This step provides an easy opportunity to begin a dialogue into potential patient concerns beyond the history.
Unfortunately, excellent bedside manner, in general, has become a rare commodity in healthcare. On a personal level, you may have experienced providers with poor bedside manners. Your experience with those providers most likely did not lead to a good provider-patient connection.
Finally, excellent clinical documentation which includes the initial personal injury patient history. This is a necessary part of all your patients’ cases. Patient history issues such as missing critical information (specific value drivers), skipping important injuries (SLAP or TBI. Including detrimental information (MPH) can be a PI practice growth obstacle.
These growth obstacles can show up in many different ways. Such as attorney reduction requests and loss of new PI patient referrals. Other examples of issues that emerge can include insurance carrier reimbursement denials or “cut-offs.”
In addition, besides the history, it is important to consider the other areas of your PI cases. All PI cases compose of several elements that continually intertwine and these can become growth obstacles as well.
Thankfully there are some practical and achievable steps you can take to get past any PI practice growth obstacle(s).
Learn More About ChiroMatrix
Would you like to learn more about how AIPIP and ChiroMatrix are working together to help chiropractors achieve their goals? Get a free website audit to learn how to improve your website and generate more personal injury patients. Identify your #1 PI practice growth obstacle, go to aipip.com right now and take our short quiz. We’ll send your results right away.